GI cocktail billing looks simple on the surface. A patient comes in with abdominal pain or heartburn. The provider orders a GI cocktail. The nurse administers it.
But billing does not work that way.
Behind the scenes, GI cocktail coding raises frequent questions for coders, billers, and even providers.
- Should it be billed as a procedure?
- Is it bundled?
- Can drugs be billed separately?
- Does route of administration matter?
- What does Medicare allow versus commercial plans?
If these questions are not handled correctly, claims get denied, bundled, or underpaid. Over time, that lost revenue adds up.
This guide explains GI cocktail coding and billing from start to finish, helping providers bill it correctly and receive timely reimbursements from insurance payers.
What is GI Cocktail Billing?
Let’s start with the basics and understand what a GA Cocktail is in a medical billing scenario.
| A GI (Gastrointestinal) Cocktail is a blend of liquid antacid, viscous lidocaine (a numbing agent), and often an antispasmodic like Donnatal (atropine, scopolamine, etc.). It is used in emergency rooms to rapidly treat indigestion (dyspepsia) or chest/belly pain. The purpose is to eliminate acid and relax the intestinal tract for relief. Studies indicate that it may not be much more effective than standard antacids in ruling out cardiac pain; however, it provides multi-symptomatic relief by decreasing acidity, alleviating pain, and mitigating spasms. |
A GI cocktail is not a single medication. It is a compound treatment, typically mixed on-site, to relieve gastrointestinal symptoms quickly.
Most GI cocktails include:
- An antacid to neutralize stomach acid
- Viscous lidocaine to numb the esophagus and stomach lining
- Sometimes an antispasmodic or anticholinergic agent
The exact formulation varies by facility. Emergency departments may use one formula, while urgent care centers or outpatient clinics use another. Some practices use premixed solutions, while others mix medications at the provider’s preference.
From a billing perspective, this matters because payer reimbursement depends on how the medication is classified, how it is administered, and whether it is considered integral to the visit.
Why GI Cocktail Billing Is a Gray Area
Medical coding systems rely on standardization. GI cocktails, by nature, are not standardized.
There is:
- No fixed drug name
- No uniform dosage
- No consistent route of administration
- No FDA-approved product
As a result, payers do not recognize GI cocktails as a separately billable service. Instead, they view them as supportive or incidental care that accompanies evaluation and management.
Coders who attempt to force GI cocktails into unrelated codes often trigger denials or audits.
GI Cocktail Reimbursement Using an Unlisted Code
When providers reach the limits of standard coding options for GI cocktail administration, unlisted procedure codes often come into play. This path exists for a reason. Medicine evolves faster than coding systems. New treatments, compounded therapies, and mixed drug administrations routinely fall into gaps where no precise CPT or HCPCS code applies.
GI cocktail administration is a textbook example of this gap.
That said, using unlisted codes is never simple, automatic, or guaranteed. It is a deliberate billing strategy that requires judgment, documentation, and realistic expectations.
Why Unlisted Procedure Codes Come into Play for GI Cocktails
A GI cocktail is not a single drug. It is not a defined procedure. It is a clinically accepted treatment that combines multiple oral medications into one administration.
Because of this, coders quickly discover three hard truths:
- No CPT code describes GI cocktail administration
- Individual drug billing usually fails due to self-administered drug rules
- Catch-all supply or drug codes are frequently denied
When all defined options fail, unlisted procedure codes are the only remaining tools that even attempt to reflect the service provided.
Unlisted codes exist to signal one thing to payers:
This service was medically necessary, performed correctly, and lacks a specific code today.
Understanding What Unlisted Codes Actually Represent
Unlisted procedure codes are not shortcuts. They do not describe a service in detail on their own.
Instead, they tell the payer, “Look at the documentation. The story is there.”
For GI cocktail administration, an unlisted code may be used to represent the clinical effort, preparation, administration, and monitoring involved when standard coding options do not apply.
However, payers expect the provider to prove why no existing code fits.
That burden always falls on documentation.
When Using an Unlisted Code May Be Reasonable
Unlisted procedure codes should never be the default choice. They may be reasonable only under specific circumstances.
For example, a provider may consider an unlisted code when:
The GI cocktail was central to patient evaluation, not incidental
Symptoms were severe or typical.
The administration required monitoring or reassessment.
The service went beyond routine office care.
In these cases, the GI cocktail is not simply comfort care. It plays a role in diagnosis or clinical decision-making.
Even then, success depends on payer policy and the strength of documentation.
GI Cocktail Ingredients and Their Impact on Care and Coding
Across the U.S., providers see gastrointestinal complaints every single day. Patients walk in with burning pain, upper abdominal discomfort, bloating, nausea, or chest pain that feels scary but turns out to be digestive in nature. In these moments, the GI cocktail becomes a practical clinical tool. It calms symptoms quickly and helps providers decide the next step in care.
But behind this simple mixture sits a layered clinical and billing reality. Each ingredient plays a specific role in symptom relief, and, from a coding perspective, each ingredient adds complexity. Understanding what goes into a GI cocktail is essential not only for treatment but also for compliant documentation and billing decisions.
Why GI Cocktails Are Common in U.S. Clinical Practice
GI complaints account for millions of outpatient and emergency visits every year in the U.S. Studies estimate that GERD and dyspepsia alone affect over 60 million Americans annually, making them some of the most common non-emergent complaints in urgent care and emergency departments.
A GI cocktail allows providers to do two things at once. First, it offers fast symptom relief. Second, it acts as a diagnostic aid. If pain improves significantly after administration, it supports a gastrointestinal origin rather than a cardiac or pulmonary cause.
Because of this dual role, GI cocktails are widely used in offices, urgent care centers, and ERs. Yet despite their commonness, coding guidance remains limited and often misunderstood.
Core Ingredients of a GI Cocktail and Their Clinical Purpose
A standard GI cocktail usually contains three categories of medication. While formulations may vary by facility or provider preference, the intent remains the same.
Liquid Antacid: Neutralizing Excess Stomach Acid
The foundation of the GI cocktail is the liquid antacid. This component neutralizes gastric acid, which is often the primary cause of burning pain and irritation.
Common antacids include aluminum hydroxide and magnesium hydroxide, which are often combined in products such as Mylanta or Maalox. These agents raise the pH of stomach contents, reducing acidity and providing rapid relief.
Simethicone is sometimes included to reduce gas bubbles, easing bloating and pressure. This does not treat acid directly but improves overall comfort.
From a coding perspective, antacids are oral, self-administered drugs. Even when given in-office, they are typically considered non-reimbursable as separate line items under most payer rules.
Viscous Anesthetic: Soothing the Inflamed GI Lining
The second key ingredient is a viscous anesthetic, most often lidocaine viscous, known by brand names such as Xylocaine viscous.
This medication coats the throat, esophagus, and stomach lining. It numbs irritated mucosa and temporarily reduces pain signals. Patients often describe a noticeable improvement within minutes.
Chemically, lidocaine works by blocking sodium channels in nerve endings. This prevents pain signals from traveling to the brain.
Although lidocaine injections are billable in many settings, oral viscous lidocaine is treated very differently. When swallowed as part of a GI cocktail, it is categorized as a self-administered oral medication. That distinction is crucial for billing and reimbursement.
Anticholinergic Agent: Reducing Spasms and Cramping
The third component targets smooth muscle activity. Anticholinergic agents such as Donnatal or glycopyrrolate are added to reduce gastrointestinal spasms and cramping.
These drugs block acetylcholine, a neurotransmitter that stimulates muscle contractions in the GI tract. By calming muscle activity, they help relieve cramping, urgency, and discomfort.
Clinically, this can make a significant difference for patients with gastritis or functional GI pain. From a billing standpoint, however, these medications remain oral and self-administered, which again limits separate reimbursement options.
GI Cocktail Composition and Dosing
While exact formulations vary, a commonly used GI cocktail includes the following components:
| Ingredient | Function | Common Brand Name | Typical Dose |
| Liquid Antacid | Neutralizes stomach acid | Mylanta or Maalox | 30 mL |
| Viscous Anesthetic | Numb throat, esophagus, stomach | Xylocaine viscous | 5 mL |
| Anticholinergic | Relieves cramping and spasms | Donnatal | 10 mL |
These medications are mixed and given orally, often in a single cup. The patient drinks the mixture under supervision.
How Ingredients Affect Coding and Billing Decisions
This is where many practices struggle.
Coding is not based on what medications were mixed. It is based on how they were administered and how payers classify them.
Even though each ingredient has its own pharmacologic identity, once combined and given orally, the GI cocktail becomes a bundled, self-administered treatment.
This distinction drives several key billing outcomes:
- The ingredients cannot usually be billed separately
- HCPCS drug codes rarely apply
- Reimbursement is expected to be included in the E/M service
Payers focus less on chemistry and more on the administration route and setting.
GI Cocktail Billing and Coding: Step-by-Step Process
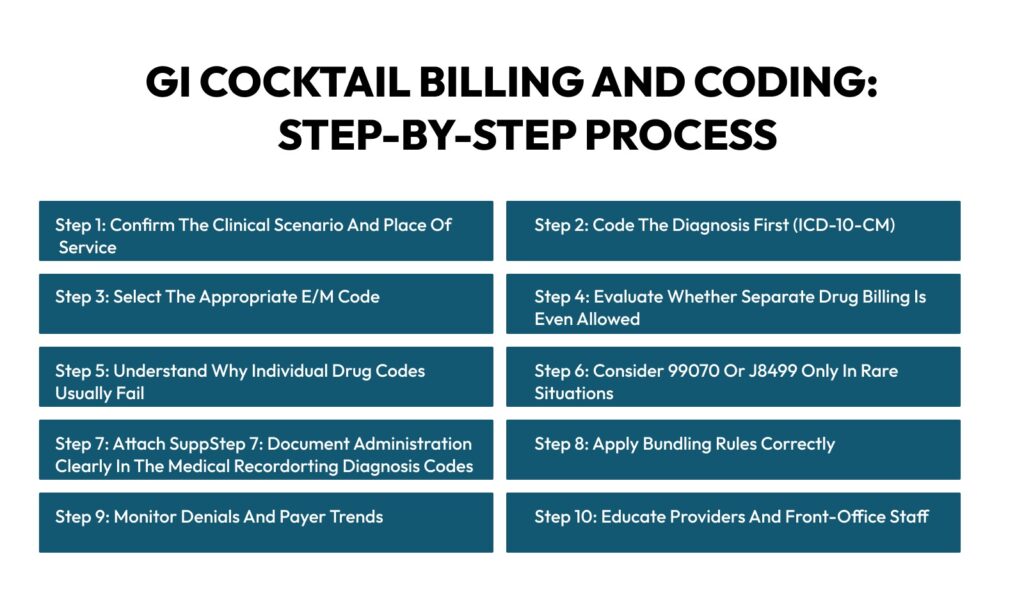
Billing a GI cocktail is not about finding a magical code. It is about understanding how payers view oral medications, how services are bundled into E/M visits, and how documentation supports the services you bill for. Below is the real, step-by-step workflow experienced billing teams follow to stay compliant and avoid denials.
This is not a theory. This is how it works in day-to-day U.S. medical billing.
Step 1: Confirm the Clinical Scenario and Place of Service
Before you even think about codes, look at where and why the GI cocktail was given.
GI cocktails are most commonly administered in:
- Physician offices
- Urgent care centers
- Emergency departments
- Gastroenterology clinics
Place of service matters because payer rules differ for office visits versus hospital-based encounters. Medicare, for example, applies stricter rules for self-administered drugs in outpatient settings.
At this step, confirm that the GI cocktail was given as part of evaluation for dyspepsia, epigastric pain, gastritis, or related symptoms, not as a standalone service.
This confirmation sets expectations early. In most cases, you are already dealing with a bundled service.
Step 2: Code the Diagnosis First (ICD-10-CM)
Diagnosis drives everything.
Start by assigning the most accurate ICD-10 code based on provider documentation. Common examples include dyspepsia, epigastric pain, GERD, or gastritis.
Avoid vague or unspecified diagnoses when possible. Payers review diagnoses to justify medical necessity. A GI cocktail given for chest pain evaluation, for example, carries a different clinical weight than one given for routine indigestion.
Clean diagnosis coding supports the E/M service, which is where reimbursement usually lives.
Step 3: Select the Appropriate E/M Code
This is the most crucial billing step.
Since GI cocktails are typically bundled, the evaluation and management code becomes the primary revenue driver.
Code the visit based on:
- Medical decision-making
- Time, if appropriate
- Complexity of symptoms
Documented assessment, differential diagnosis, and response to treatment matter here.
A patient presenting with severe epigastric pain, requiring diagnostic evaluation and symptom relief, may justify a higher-level E/M than simple indigestion.
This is where experienced coders protect revenue without violating payer rules.
Step 4: Evaluate Whether Separate Drug Billing Is Even Allowed
Now comes the critical judgment call.
Ask one question:
Is the GI cocktail a self-administered oral drug?
In almost all cases, the answer is yes.
Under Medicare and most commercial plans, self-administered oral medications are not separately reimbursed when provided in an office or outpatient setting.
At this step, many billing teams intentionally stop. They do not attempt separate drug billing because experience shows it leads to denials.
Knowing when not to bill is a skill.
Step 5: Understand Why Individual Drug Codes Usually Fail
Each component of a GI cocktail has its own classification. But once mixed and given orally, payers no longer treat them as billable injections or infusions.
You cannot realistically bill:
- Antacid components
- Viscous lidocaine orally
- Antispasmodics orally
Even if prepared by staff, they fall under self-administered drug rules.
Trying to break them out often triggers payer edits and denials.
Step 6: Consider 99070 or J8499 Only in Rare Situations
Some providers still ask about alternative codes.
CPT 99070 for supplies may be considered, but most payers either bundle it or deny it because medications are not regarded as incidental supplies.
HCPCS J8499 for unclassified oral drugs is another option, usually in ASC or hospital settings. However, this code almost always requires manual review and extensive documentation.
Use these codes only if:
- A payer policy explicitly allows it
- The provider understands the denial risk
- Documentation is robust
Otherwise, they create more work than they return.
Step 7: Document Administration Clearly in the Medical Record
Even when you do not bill separately, documentation still matters.
The provider should clearly document:
- Reason for GI cocktail administration
- Symptoms and clinical findings
- Medications and dosages used
- Patient response to treatment
This documentation supports the medical necessity of the E/M visit and protects the practice during audits.
Clear notes also help justify higher-level E/M codes when appropriate.
Step 8: Apply Bundling Rules Correctly
Bundling is not a penalty. It is how payers structure reimbursement.
GI cocktails are generally considered incidental to evaluation and treatment.
The cost is expected to be covered under:
- Office visit payment
- Emergency department E/M
- Procedure global package
Applying bundling correctly prevents compliance issues and overbilling risks.
Step 9: Monitor Denials and Payer Trends
Even when billing correctly, payer behavior changes.
Experienced billing teams regularly review denial patterns. If a payer begins paying or denying inconsistently, document it.
Patterns matter more than one-off payments.
Use denial data to guide future billing decisions instead of reacting claim by claim.
Step 10: Educate Providers and Front-Office Staff
Many billing problems start upstream.
Providers sometimes expect separate reimbursement because medication was given. Front-desk staff may assume drug charges apply.
Education closes this gap.
When everyone understands that GI cocktails are usually bundled, expectations align, and billing becomes smoother.
Final Thoughts
GI cocktail administration falls into a gray area of medical billing. Clinically, it is effective, fast, and widely accepted. From a coding and reimbursement standpoint, however, it demands caution, clarity, and strong documentation. There is no single CPT or HCPCS code that perfectly captures a GI cocktail. Most payers view it as a bundled, self-administered oral treatment tied to the evaluation and management service.
Providers who expect separate reimbursement often face denials. Those who document thoroughly, code conservatively, and understand payer expectations avoid audits and compliance headaches. The real opportunity lies in optimizing the E/M level, supporting medical necessity, and applying unlisted codes only when absolutely justified.
In short, GI cocktail billing is less about chasing a perfect code and more about mastering documentation, payer rules, and revenue cycle discipline. Practices that treat it this way stay compliant and financially stable.
Turn Coding Gray Areas into Clean Revenue
Medhesty Medical Billing helps practices navigate complex scenarios, such as GI cocktail coding, with clarity and compliance. Our team understands payer rules, Medicare policies, and real-world denial trends. We focus on protecting revenue without triggering audits.
Whether you run a physician’s office, urgent care center, or outpatient facility, Medhesty ensures your GI services are coded accurately, appropriately documented, and reimbursed correctly—every time.
FAQs
Is there a specific CPT or HCPCS code for a GI cocktail?
No. There is currently no dedicated CPT or HCPCS code that represents a GI cocktail as a single service. Each ingredient may have its own drug identity, but when combined and given orally, payers treat it as a bundled service. Most reimbursement is tied to the E/M visit rather than the medications themselves.
Can CPT code 99070 be used to bill for a GI cocktail?
Some practices attempt to use 99070 for supplies and materials, but this code is not intended for medications. Most commercial payers and Medicare deny claims when 99070 is used for GI cocktails. It should be used cautiously and only when payer policy explicitly allows it.
Does Medicare reimburse for GI cocktail administration?
In most outpatient settings, Medicare considers GI cocktail components to be self-administered oral drugs. These are generally non-covered. Medicare expects the cost to be bundled into the E/M service, making separate reimbursement unlikely.
When should unlisted procedure or drug codes be considered?
Unlisted codes may be considered when no existing code reasonably describes the service and when medical necessity is clearly documented. Even then, prior authorization, detailed narratives, and follow-up are essential. Payment is never guaranteed, and denial rates are high without payer approval.
What documentation is essential for GI cocktail billing?
Strong documentation should include presenting symptoms, clinical rationale for administration, exact medications and dosages, route of administration, and patient response. This supports E/M coding, demonstrates medical necessity, and protects the practice during audits or payer reviews.



