Anxiety disorders are among the most common mental health diagnoses in the United States, representing a significant portion of behavioral health billing. According to recent surveys, more than 20% of adults experience an anxiety disorder each year, and practices are increasingly relying on ICD-10 codes to capture these diagnoses accurately. For mental health providers, correct coding is not just about compliance; it directly impacts reimbursement, claim acceptance, and revenue stability.
In this guide, we’ll cover everything from ICD-10 code selection and documentation requirements to CPT coding, payer-specific strategies, and reimbursement optimization for anxiety treatment. By the end, your practice will have a roadmap for accurately coding, documenting, and billing for anxiety services while reducing denials.
Quick Anxiety ICD-10 Code Lookup
Behavioral health billers and clinicians often need a fast reference. Below is a practical snapshot of the most commonly used anxiety ICD-10-CM codes and what payers expect in documentation.
| Disorder | ICD-10 Code | Core Criteria | Documentation Focus |
|---|---|---|---|
| Generalized Anxiety Disorder | F41.1 | ≥6 months excessive worry | 3+ physical symptoms + impairment |
| Panic Disorder | F41.0 | Recurrent unexpected attacks | 4+ panic symptoms + 1 month behavior change |
| Social Anxiety Disorder (Generalized) | F40.11 | Social fear across most settings | 6+ months + avoidance |
| Agoraphobia | F40.0 | Fear of escape difficulty | Avoidance + companion reliance |
| Adjustment Disorder w/ Anxiety | F43.22 | Stressor within 3 months | Named stressor + proportionality |
| Adjustment Disorder w/ Mixed Anxiety & Depression | F43.23 | Anxiety + depressive symptoms | Timeline + dual symptom documentation |
| PTSD | F43.10 | Trauma + 4 symptom clusters | Trauma exposure + functional impact |
This table improves claim accuracy and reduces overuse of unspecified codes like F41.9.
Understanding Anxiety Disorder Coding
Anxiety disorders are coded primarily under ICD-10 categories F40–F48, which encompass:
- Phobic anxiety disorders (F40)
- Other anxiety disorders (F41)
- Obsessive-compulsive and related disorders (F42)
- Stress-related and adjustment disorders (F43)
Proper coding ensures that diagnoses are trackable, clinically justified, and reimbursable. Missteps, such as using unspecified codes (e.g., F41.9) or failing to document functional impairment, lead to denials and audit triggers. Studies show that 15–25% of mental health claim denials are linked directly to vague or incorrect ICD-10 documentation.
Effective October 1, 2025, the FY 2026 ICD-10 updates refine anxiety coding, expanding specificity for generalized anxiety disorder, panic disorder, and adjustment disorders. Practices must integrate these changes into electronic health records, superbills, and staff training to maintain compliance and reimbursement efficiency.
Anxiety ICD-10 Categories and Clinical Overview
F40 – Phobic Anxiety Disorders
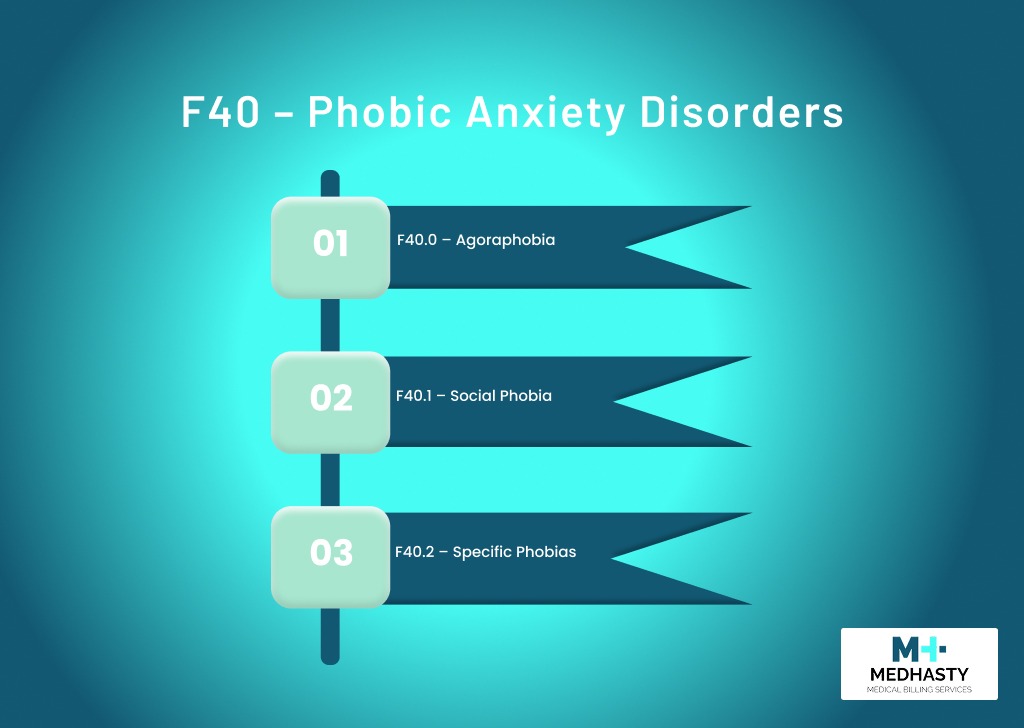
Phobic disorders are marked by excessive fear of specific objects or situations, leading to avoidance and functional impairment. Proper documentation is critical, particularly for social phobias, agoraphobia, and specific phobias.
- F40.0 – Agoraphobia: Fear of situations where escape might be difficult
- F40.1 – Social Phobia: Anxiety in social interactions with potential scrutiny
- F40.2 – Specific Phobias: Isolated fears, such as arachnophobia, claustrophobia, or fear of flying
Documentation must include: duration of at least six months, functional impairment, avoidance behavior, and physical anxiety symptoms.
F41 – Other Anxiety Disorders
This category is the most frequently billed in behavioral health:
- F41.0 – Panic Disorder: Recurrent unexpected panic attacks
- F41.1 – Generalized Anxiety Disorder (GAD): Chronic, excessive worry with physical and cognitive symptoms
- F41.3 – Other Mixed Anxiety Disorders
- F41.8 – Other Specified Anxiety Disorders
- F41.9 – Anxiety Disorder, Unspecified
Correct code selection requires matching DSM-5 criteria with documented symptom frequency, duration, and severity.
F42 – Obsessive-Compulsive Disorders
Although OCD is a distinct category, it often coexists with anxiety. Coding should accurately reflect primary and secondary diagnoses, especially when billing for therapy or medication management.
F43 – Reaction to Severe Stress and Adjustment Disorders
- F43.0 – Acute Stress Reaction: Immediate response to a traumatic event, typically short-term
- F43.1 – Post-Traumatic Stress Disorder (PTSD): Must document trauma exposure and symptom clusters
- F43.22 – Adjustment Disorder with Anxiety
- F43.23 – Adjustment Disorder with Mixed Anxiety and Depressed Mood
For these codes, timeline documentation, identifiable stressors, and functional impact are critical for payer approval.
Most Commonly Used Anxiety ICD-10 Codes
Based on practice patterns and payer analysis, the top 5 anxiety codes are:
| ICD-10 | Disorder | Documentation Focus |
| F41.1 | Generalized Anxiety Disorder | Chronic worry, ≥3 physical symptoms, functional impairment |
| F41.9 | Anxiety Disorder, Unspecified | Initial assessments, significant anxiety not yet fully evaluated |
| F41.0 | Panic Disorder | ≥4 panic symptoms per episode, behavioral changes |
| F43.23 | Adjustment Disorder with Mixed Anxiety & Depressed Mood | Stressor identification, combined with symptom documentation |
| F40.10 | Social Phobia, Unspecified | Social situation avoidance, anxiety triggers |
Code Breakdowns and Documentation Essentials
F40 Series – Phobic Anxiety Disorders
Phobic anxiety disorders involve intense fear or anxiety about specific situations or objects. Patients often avoid triggers, and the fear causes measurable disruption to daily life. Documentation is critical because phobias can overlap with other anxiety disorders; payers want proof that the phobia is clinically significant.
F40.0 – Agoraphobia
Fear of places or situations where escape might be intricate, or help might not be available if panic-like symptoms occur. Examples include open spaces, crowded areas, public transportation, or enclosed spaces.
Key Documentation:
- Identify the exact situations that trigger fear.
- Document avoidance behaviors (e.g., refuses public transit or requires a companion).
- Duration ≥ 6 months. Shorter durations may not meet diagnostic criteria.
- Note functional impairment in social, work, or home settings.
Why it matters: Agoraphobia often leads to multiple missed visits or therapy sessions, so proper coding ensures therapy and evaluation are reimbursable.
F40.1 – Social Phobias (Social Anxiety Disorder)
Fear of negative evaluation in social or performance situations. Examples: public speaking, meeting new people, and social gatherings.
Key Documentation:
- List specific social triggers.
- Describe how social interactions provoke nearly constant fear or anxiety.
- Duration ≥ 6 months.
- Impairment in work, school, or social relationships must be clearly noted.
Specificity is essential—use F40.10 for unspecified social phobia, F40.11 for generalized social phobia affecting most interactions.
F40.2 – Specific Phobias
Anxiety focused on a single object or situation (animals, heights, medical procedures, blood).
Key Documentation:
- The immediate fear response must be described.
- Avoidant behaviors or intense distress must be documented.
- Duration ≥ 6 months.
- Functional or emotional distress must be clinically significant.
CPT billing for therapy or desensitization interventions depends on documenting functional impairment, not just fear.
F41 Series – Other Anxiety Disorders
F41 codes cover generalized anxiety, panic disorders, and mixed anxiety presentations. They are the most frequently billed anxiety codes in mental health practices.
F41.0 – Panic Disorder
Recurrent, unexpected panic attacks, often accompanied by persistent worry about additional attacks and behavior changes.
Key Documentation:
- Document at least 4 panic symptoms (palpitations, sweating, chest pain, dizziness, etc.).
- Behavioral changes lasting ≥ 1 month after attacks (avoidance, lifestyle changes).
- Confirm attacks are not due to substances or medical conditions.
CPT psychotherapy codes are billable if the clinical documentation supports treatment of panic disorder.
F41.1 – Generalized Anxiety Disorder (GAD)
Chronic, excessive worry on most days for ≥ 6 months.
Key Documentation:
- Difficulty controlling worry.
- At least 3 physical or cognitive symptoms: restlessness, fatigue, concentration problems, irritability, muscle tension, sleep disturbances.
- Functional impairment in work, social, or home life.
GAD is the most commonly billed anxiety disorder; precise documentation improves payer acceptance and reduces the risk of denials.
F41.8 – Other Specified Anxiety Disorders
Anxiety that doesn’t fit into specific categories but can be described in clinical notes.
Clearly specify what features are present and why other codes are not applicable.
F41.9 – Anxiety Disorder, Unspecified
- For early visits, emergencies, or when insufficient information exists.
- Use only temporarily; persistent use may trigger audit risk. F41.8 is preferred if any specificity exists.
F43 Series – Stress and Adjustment Disorders
F43 codes are used when anxiety is linked to a specific stressor or trauma. These disorders often involve both anxiety and depression, requiring careful documentation to support medical necessity.
F43.22 – Adjustment Disorder with Anxiety
Emotional or behavioral symptoms arise within 3 months of an identifiable stressor (e.g., job loss, divorce).
Key Documentation:
- Identify the stressor clearly.
- Describe anxiety symptoms and their functional impact.
- Ensure distress is out of proportion to the stressor.
F43.23 – Adjustment Disorder with Mixed Anxiety and Depressed Mood
Both anxiety and depressive symptoms are present due to a stressor.
Key Documentation:
- Both symptom types must be clearly documented.
- Timeline of symptom onset and resolution.
- Functional impairment noted.
- Symptoms generally resolve within 6 months after the stressor ends.
Because these codes are often secondary diagnoses, linking therapy or evaluation services to the primary stressor improves claim approval rates.
DSM-5 vs ICD-10 Crosswalk for Anxiety Disorders
While claims are submitted using ICD-10-CM codes, diagnoses are established using DSM-5-TR criteria. Payers often review documentation to ensure the ICD-10 code is supported by DSM criteria.
For example:
- Generalized Anxiety Disorder (F41.1) requires excessive anxiety occurring more days than not for at least 6 months, plus at least three associated symptoms.
- Panic Disorder (F41.0) requires recurrent unexpected panic attacks and persistent concern about additional attacks.
- Social Anxiety Disorder (F40.11) requires marked fear of social situations involving scrutiny and avoidance lasting at least 6 months.
If DSM criteria are not clearly documented, payers may argue lack of medical necessity — even if the correct ICD-10 code was selected.
Best Practice:
Document DSM symptom criteria explicitly in your assessment. This strengthens compliance, supports audits, and protects reimbursement.
CPT Codes for Anxiety Treatment
Evaluation Codes
| CPT | Description | Use Case |
| 90791 | Psychiatric evaluation (no meds) | Initial therapy assessment |
| 90792 | Psychiatric evaluation with medical services | Intake with medication management |
Psychotherapy Codes (Time-Based)
| CPT | Duration | Use |
| 90832 | 16–37 min | Brief individual therapy |
| 90834 | 38–52 min | Standard individual therapy |
| 90837 | 53+ min | Extended individual therapy |
Add-On Codes
| CPT | Description | Use |
| 90785 | Interactive complexity | For patients with barriers to communication |
| 90833/90836/90838 | Psychotherapy with E/M | When therapy coincides with evaluation or management |
Group and Family Therapy Codes
| CPT | Description |
| 90846 | Family therapy, patient not present |
| 90847 | Family therapy, patient present |
| 90849 | Multi-family group therapy |
| 90853 | Group therapy (non-family) |
Crisis Intervention
| CPT | Duration |
| 90839 | First 60 min |
| 90840 | Each additional 30 min |
Documentation must include: crisis assessment, mental status exam, disposition, and recommendations.
Telehealth Billing for Anxiety Disorders (2026 Updates)
Telehealth has become a primary delivery model for anxiety treatment. However, billing requirements vary by payer.
Place of Service (POS)
- POS 02 – Telehealth provided other than in patient’s home
- POS 10 – Telehealth provided in patient’s home
Required Modifiers
- Modifier 95 – Synchronous telemedicine service
- Modifier GT – Used by certain commercial payers
Medicare Considerations
Medicare continues to reimburse tele-mental health services, but documentation must include:
- Confirmation of patient consent
- Technology used
- Provider and patient locations
- Confirmation service was real-time audio/video
Audio-only services may be limited by payer and state.
Common Telehealth Error:
Failing to document that the encounter was conducted via real-time interactive communication technology.
Proper telehealth coding significantly reduces denial rates for anxiety therapy claims.
Documentation Best Practices
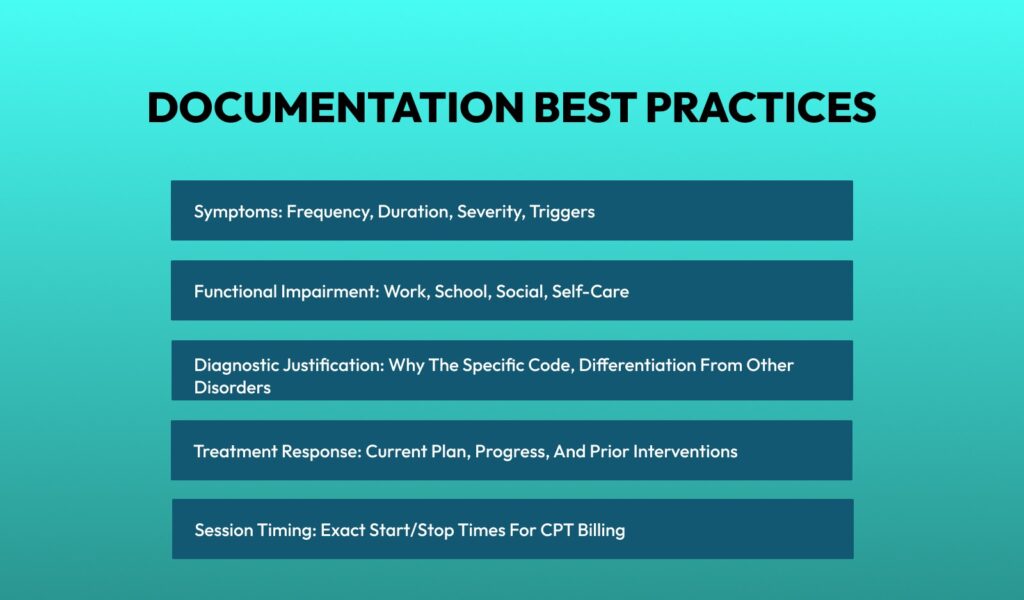
Essential Elements
- Symptoms: Frequency, duration, severity, triggers
- Functional Impairment: Work, school, social, self-care
- Diagnostic Justification: Why the specific code, differentiation from other disorders
- Treatment Response: Current plan, progress, and prior interventions
- Session Timing: Exact start/stop times for CPT billing
Pro Tip: Use structured templates for consistency across providers and visits.
Common Comorbidities With Anxiety Disorders
Anxiety rarely exists in isolation. Proper sequencing and documentation of comorbid conditions improves reimbursement accuracy and clinical representation.
Major Depressive Disorder (F32/F33)
Frequently co-occurs with GAD and panic disorder. If both conditions are actively treated, they should be coded separately.
Substance Use Disorders (F10–F19)
Substances may exacerbate anxiety symptoms. Document whether anxiety is primary or substance-induced.
Insomnia (G47.00)
Sleep disturbance is a core anxiety symptom, but if treated independently, it may be coded separately.
ADHD (F90.9)
In adults, ADHD and anxiety commonly overlap. Clarify diagnostic differentiation in documentation.
Somatic Symptom Disorder (F45.1)
Important when anxiety presents primarily with physical complaints.
Sequencing Rule:
List the primary reason for the visit first. Secondary diagnoses should reflect active treatment relevance.
Proper comorbidity coding strengthens medical necessity and reduces payer scrutiny.
Common Coding Errors and How to Avoid Them
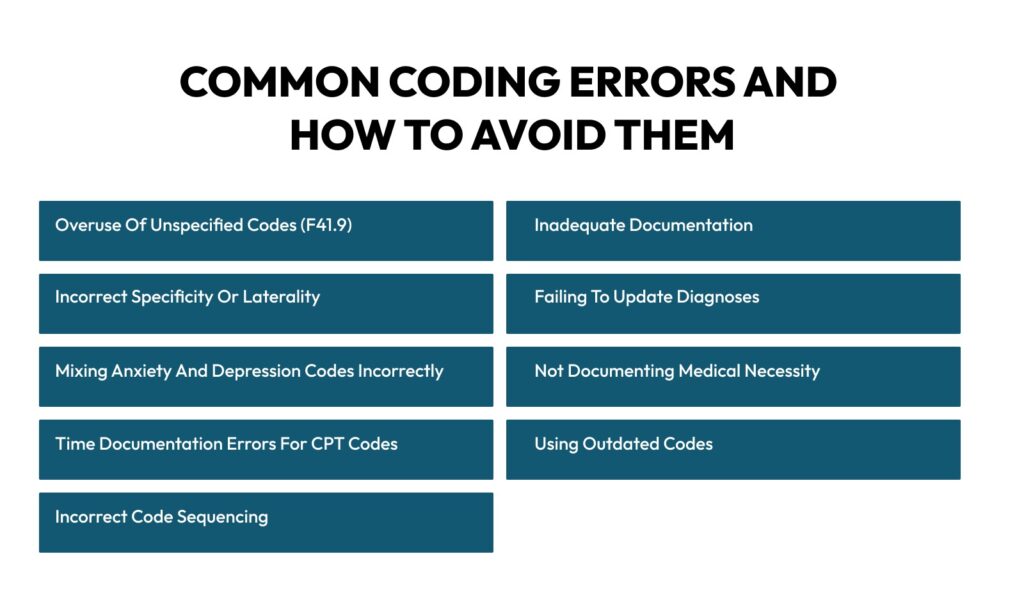
Anxiety disorder coding is deceptively tricky. Even small mistakes—such as using the wrong ICD-10 code or incomplete documentation—can lead to claim denials, audit flags, or underpayments. By understanding the common pitfalls, practices can create robust workflows and avoid repeated mistakes.
Overuse of Unspecified Codes (F41.9)
Billing F41.9 (Anxiety Disorder, Unspecified) by default instead of a more precise code, such as F41.1 (GAD) or F41.0 (Panic Disorder).
- Clinicians may use unspecified codes when the assessment is incomplete or when anxious patients present with mixed symptoms.
- Staff may choose unspecified codes to “save time” on documentation.
How to avoid:
- Conduct thorough assessments before coding.
- Update the diagnosis once a specific disorder is identified.
- Use F41.8 (Other Specified Anxiety Disorder) when partial specificity exists.
Inadequate Documentation
Using vague statements like “patient anxious” without specifying symptoms, duration, or functional impact.
- Claims may be rejected for lack of medical necessity.
- Clinical notes may fail audits or payer review.
- Reduces data quality for outcome tracking and reporting.
How to avoid:
- Document specific symptoms (e.g., restlessness, sleep disturbance, palpitations).
- Include frequency, duration, and triggers.
- Note functional impairment in work, social, or daily activities.
Incorrect Specificity or Laterality
Using codes that are too general, like F40.10 (Social Phobia, Unspecified) when generalized social anxiety (F40.11) is present.
- Undercoding reduces reimbursement.
- Misrepresents the clinical picture.
- May cause repeated edits during audits.
How to avoid:
- Match the ICD-10 code to the full clinical presentation.
- Update codes as the patient’s condition evolves.
Failing to Update Diagnoses
Continuing to bill “unspecified” codes throughout treatment, even after the assessment clarifies the disorder.
- Audit risk increases.
- Documentation appears incomplete.
- Payers may delay or deny claims.
How to avoid:
- Review diagnoses periodically, especially after initial evaluation.
- Update the patient record as soon as the specific anxiety disorder is confirmed.
Mixing Anxiety and Depression Codes Incorrectly
Billing only an anxiety code when depression is also present, or incorrectly sequencing adjustment disorder with mixed anxiety and depression.
- Reimbursement may be inaccurate.
- The clinical record doesn’t fully reflect the patient’s status.
- May trigger payer review for incomplete coding.
How to avoid:
- Code anxiety and depression separately when clinically indicated.
- Use F43.23 for adjustment disorders with both anxiety and depressive symptoms.
- Include proper sequencing and documentation for combined presentations.
Not Documenting Medical Necessity
Billing psychotherapy or evaluation CPT codes without connecting the ICD-10 diagnosis to medical necessity.
- Denied claims.
- Increased audits and compliance risks.
How to avoid:
- Clearly link each billed service to the patient’s ICD-10 diagnosis.
- Include treatment goals and clinical rationale in the note.
- Demonstrate ongoing need and progress monitoring.
Time Documentation Errors for CPT Codes
Not recording start and stop times accurately for time-based psychotherapy codes (90832, 90834, 90837). Rounding or estimating session times.
- Fraud concerns.
- Claim denials or recoupments.
- Reduced revenue for longer therapy sessions.
How to avoid:
- Document exact start and end times.
- Only bill for face-to-face time with the patient.
- Avoid rounding; follow payer rules strictly.
Using Outdated Codes
Billing codes from prior ICD-10-CM versions, or not updating after the October 1 ICD-10 annual updates.
- Automatic claim rejections.
- Delayed payments.
- Noncompliance risk.
How to avoid:
- Review annual ICD-10 updates before each fiscal year.
- Update EMR templates and superbills.
- Train staff on new codes and revisions.
Incorrect Code Sequencing
Listing secondary or less relevant diagnoses as the primary code.
- Reimbursement may be reduced.
- Payers may question the medical necessity of services.
- Data tracking for quality reporting is compromised.
How to avoid:
- Always list the primary reason for the visit first.
- Include relevant comorbidities in secondary positions.
- Align documentation with code sequencing.
Frequently Asked Questions (FAQ)
What is the ICD-10 code for anxiety?
The general code for unspecified anxiety disorder is F41.9. However, F41.1 (GAD) or F41.0 (Panic Disorder) should be used when criteria are met.
What is the ICD-10 code for Generalized Anxiety Disorder?
F41.1.
What is the ICD-10 code for Panic Disorder?
F41.0.
What is the ICD-10 code for Adjustment Disorder with Anxiety?
F43.22.
Can anxiety and depression be coded together?
Yes. If both conditions are documented and actively treated, they should be coded separately unless using F43.23 for adjustment disorder with mixed features.
How long must anxiety symptoms last to diagnose GAD?
Symptoms must persist for at least six months.
Conclusion
Accurate coding for anxiety disorders requires clinical understanding, detailed documentation, and awareness of compliance requirements. By:
- Using specific ICD-10 codes
- Documenting symptoms, duration, and functional impairment
- Aligning CPT billing with face-to-face time
- Tracking updates annually\
Behavioral health providers can reduce denials, improve revenue, and maintain compliance. Anxiety coding is more than a formality—it’s the foundation for accurate reimbursement and quality care tracking.
Struggling with anxiety claim denials or inconsistent reimbursements?
Medhasty’s behavioral health billing specialists help practices improve clean claim rates, strengthen documentation, and reduce audit exposure.
Schedule your free billing assessment today and protect your revenue cycle.