Sleep apnea is no longer a niche diagnosis.
It is now one of the most frequently documented sleep-related disorders across primary care, pulmonology, cardiology, neurology, ENT, and sleep medicine practices in the United States.
Yet, despite its prevalence, sleep apnea claims continue to face high denial rates, delayed payments, and audit risk. The reason is not the condition itself. The problem lies in how ICD-10 codes for sleep apnea are selected, documented, and billed.
Many practices underestimate how closely payers examine sleep apnea diagnoses. Others rely on generic coding habits that worked years ago but no longer meet today’s payer standards.
This guide explains ICD-10 sleep apnea codes the way real billing teams and providers need to understand them. It connects clinical documentation, diagnostic testing, payer rules, and reimbursement expectations into one clear picture.
Who This Guide Is For
This guide is designed for healthcare professionals and billing teams who manage sleep apnea services and need accurate, denial-resistant coding. It is particularly relevant for:
- Sleep medicine clinics and diagnostic sleep labs
- Pulmonology, cardiology, neurology, and ENT practices
- Primary care providers managing sleep disorder referrals
- Medical billing and coding teams
- DME suppliers handling CPAP and PAP therapy claims
Whether you are diagnosing sleep apnea, billing sleep studies, managing CPAP compliance, or appealing denials, accurate ICD-10 coding is the foundation of successful reimbursement.
Apnea in a Clinical and Billing Context
Sleep apnea is not a single condition.
It is a category of disorders characterized by repeated interruptions in breathing during sleep. Airway obstruction, neurologic signaling issues, or a combination of both may cause these interruptions.
From a billing perspective, this distinction is critical. Payers generally do not reimburse for “sleep apnea.” They reimburse specific types of sleep apnea supported by objective testing and medical necessity.
This is why ICD-10 coding accuracy matters so much in sleep medicine. The diagnosis drives coverage for sleep studies, CPAP therapy, DME supplies, and long-term management.
Primary ICD-10 Codes for Sleep Apnea
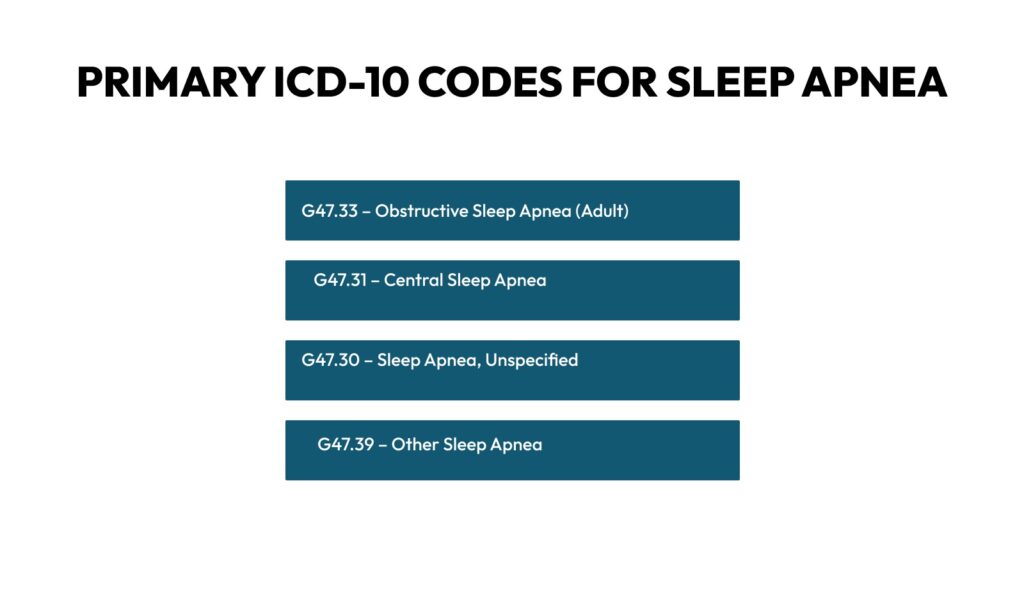
The most commonly used ICD-10 codes for sleep apnea fall under the G47.3 category. Each code reflects a different clinical mechanism, and each carries different billing implications.
G47.33 – Obstructive Sleep Apnea (Adult)
G47.33 is by far the most frequently billed sleep apnea diagnosis. It describes obstructive sleep apnea in adults, where airway collapse or obstruction causes breathing pauses during sleep.
This code is widely accepted by Medicare and commercial payers when supported by a qualifying sleep study. It commonly supports reimbursement for:
- Diagnostic polysomnography
- CPAP and BiPAP therapy
- Ongoing DME supplies
Because of its prevalence, G47.33 is also heavily audited. Documentation must clearly link symptoms, testing results, and treatment decisions.
G47.31 – Central Sleep Apnea
Central sleep apnea occurs when the brain fails to send proper signals to the muscles that control breathing. It is less common than obstructive sleep apnea and often associated with neurologic disease, heart failure, or opioid use.
Claims billed with G47.31 require strong supporting documentation, as payers often scrutinize whether the diagnosis is truly central rather than obstructive.
G47.30 – Sleep Apnea, Unspecified
G47.30 is used when sleep apnea is suspected, but the type has not yet been determined. From a billing standpoint, this code should be handled with caution.
It may be appropriate during initial evaluations or referrals, but prolonged use without diagnostic clarification increases the risk. Payers expect the type of sleep apnea to be confirmed through testing.
G47.39 – Other Sleep Apnea
This code applies to less common forms of sleep apnea that do not fit neatly into obstructive or central categories. It is used sparingly and usually in complex cases.
ICD-10 Codes for Sleep Apnea – Quick Reference Table
| ICD-10 Code | Description | Billing Risk Level | Key Billing Notes |
|---|---|---|---|
| G47.33 | Obstructive Sleep Apnea (Adult) | High | Most commonly billed and audited |
| G47.31 | Central Sleep Apnea | High | Requires strong neurologic or cardiac justification |
| G47.30 | Sleep Apnea, Unspecified | Very High | Short-term use only; high denial risk |
| G47.39 | Other Sleep Apnea | Moderate | Used in rare, complex cases |
This table improves claim accuracy, speeds internal review, and reduces reliance on unspecified diagnosis codes that often trigger payer scrutiny.
Diagnostic Testing and Medical Necessity for Sleep Apnea
Sleep apnea diagnoses are not based solely on symptoms.
Payers require objective evidence.
Polysomnography and home sleep apnea testing are the foundation of diagnosis. The test results must demonstrate apnea-hypopnea index (AHI) thresholds that meet payer criteria.
Medicare, for example, requires documented AHI values and associated symptoms to support coverage for CPAP therapy. Commercial payers often follow similar standards but may impose additional requirements.
Without clear test documentation, even the correct ICD-10 code will fail to support reimbursement.
Documentation for Apnea ICD-10 Codes
Strong documentation tells a complete story.
It explains why testing was ordered, what the results show, and how treatment decisions were made.
Clinical notes should reflect:
- Daytime sleepiness or fatigue
- Snoring or witnessed apneas
- Cardiovascular or metabolic comorbidities
- Sleep study findings
- Severity classification
When documentation is vague or fragmented, payers question medical necessity. This is one of the most common causes of denied sleep apnea claims.
Common Sleep Apnea ICD-10 Coding Errors That Cause Denials
Sleep apnea denials are rarely caused by the condition itself. They are most often the result of coding and documentation errors that weaken medical necessity. The most common issues include:
- Prolonged use of G47.30 (unspecified sleep apnea) after diagnostic testing
- Missing or incomplete sleep study reports in the medical record
- CPT codes billed without a matching, specific diagnosis
- CPAP-related services billed before confirming obstructive sleep apnea
- Lack of severity classification or AHI documentation
Payers expect diagnosis codes to evolve as testing confirms the type and severity of sleep apnea. Failure to update codes increases denial risk and audit exposure.
CPT Codes Billed with Sleep Apnea Diagnoses
Sleep apnea billing is not limited to a single CPT code or service type. In real-world practice, providers bill a cluster of diagnostic, monitoring, and treatment-related CPT codes tied closely to the sleep apnea diagnosis being managed. When these codes are not linked correctly to ICD-10 sleep apnea diagnoses, claims stall, are denied, or are reimbursed at lower rates.
From my experience working with sleep clinics, pulmonology groups, ENT practices, and primary care offices, most billing issues arise when providers bill the correct service but fail to match it to the diagnosis, setting, or payer expectations. Let’s break this down in detail so you understand which CPT codes are commonly billed, why they are used, and how payers review them.
Diagnostic Sleep Study CPT Codes
Diagnostic testing forms the foundation of sleep apnea billing. Payers expect objective evidence before approving long-term therapy such as CPAP or oral appliances. Because of this, diagnostic CPT codes are heavily scrutinized.
95810 – Polysomnography (PSG), In-Lab Study
This code is used for a complete, attended overnight sleep study performed in a sleep lab. It records multiple physiologic parameters, including EEG, EOG, EMG, airflow, respiratory effort, and oxygen saturation.
Providers typically bill 95810 when:
- The patient has suspected moderate to severe sleep apnea
- Comorbid conditions exist, such as COPD, heart failure, or neurologic disorders.
- Home sleep testing is not appropriate or has been inconclusive.
Medicare and commercial payers often view 95810 as the gold standard. However, the documentation must justify why an in-lab study was medically necessary rather than a home test. Without that explanation, payers may downcode or deny the claim.
95811 – Polysomnography with CPAP/BiPAP Titration
This code applies when positive airway pressure titration is performed during the sleep study. It is commonly billed when sleep apnea has already been established, to determine optimal CPAP or BiPAP settings.
Key billing considerations include:
- Clear documentation that titration occurred
- Evidence that the patient tolerated PAP therapy
- A confirmed sleep apnea diagnosis supporting the service
Many denials occur when providers bill 95811 without documentation showing that titration was clinically indicated.
Home Sleep Testing CPT Codes
Home sleep testing has grown rapidly, especially following expanded coverage policies and the adoption of telehealth. Payers favor home testing when clinically appropriate because it is less costly than in-lab studies.
95800 – Unattended Sleep Study
This code represents a basic unattended sleep study measuring respiratory effort, airflow, and oxygen saturation.
It is commonly billed for:
- Patients with a high pre-test probability of obstructive sleep apnea
- Individuals without significant cardiopulmonary comorbidities
However, payers expect strict adherence to coverage criteria. If the patient does not meet home testing requirements, claims may be denied even if the test was performed correctly.
95806 – Home Sleep Apnea Test with Respiratory Parameters
This is one of the most frequently billed CPT codes for sleep apnea diagnostics today. It includes monitoring airflow, respiratory effort, and oxygen saturation.
Billing success depends on:
- Proper physician order
- Interpretation by a qualified provider
- Clear linkage to an appropriate sleep apnea diagnosis code
Failure to document physician interpretation is a common mistake that leads to recoupments.
Evaluation and Management (E/M) CPT Codes
Sleep apnea management does not stop at diagnosis. Ongoing evaluation, counseling, and follow-up visits are essential parts of care and are frequently billed.
99202–99205 and 99212–99215 – Office or Outpatient E/M Visits
These codes are used for new and established patient visits related to:
- Initial sleep apnea evaluation
- Review of sleep study results
- CPAP compliance discussions
- Symptom reassessment and treatment planning
Payers expect:
- A clear medical decision-making process
- Documentation of symptoms such as daytime sleepiness, snoring, or witnessed apneas
- Time or complexity justification based on current E/M guidelines
Overcoding E/M levels without adequate documentation increases audit risk, especially when sleep apnea follow-ups are billed repeatedly.
CPAP and PAP Therapy Related CPT and HCPCS Codes
Treatment of sleep apnea often involves durable medical equipment. While many of these are HCPCS codes, CPT-related services support their use and compliance with CPT.
94660 – CPAP Ventilation Assistance
This CPT code is used for continuous positive airway pressure assistance, often billed when CPAP therapy is initiated or monitored in a clinical setting.
Common billing errors include:
- Billing 94660 without documentation of hands-on assistance
- Using it repeatedly without medical necessity
- Billing on the same day as certain sleep studies without a modifier justification
Payers carefully review this code due to historical overuse.
ENT and Surgical CPT Codes Linked to Sleep Apnea
In cases where conservative therapy fails, surgical intervention may be considered. Sleep apnea diagnoses often support a variety of ENT-related CPT codes.
31575 – Diagnostic Laryngoscopy
Used to evaluate airway obstruction contributing to sleep apnea. Documentation must explain how findings relate to the apnea diagnosis.
42145 – Uvulopalatopharyngoplasty (UPPP)
A surgical treatment for obstructive sleep apnea in select patients. This code requires:
- Strong medical necessity documentation
- Prior authorization from most payers
- Evidence that non-surgical treatments were ineffective or intolerable
These claims often undergo pre- and post-payment review.
Oral Appliance Therapy Related Codes
Some patients cannot tolerate CPAP and move toward oral appliance therapy.
97760 / 97763 – Orthotic Management and Training
These CPT codes may be used for training and adjustment of oral appliances when billed by eligible providers.
Payers expect:
- Documentation that CPAP was not tolerated or contraindicated
- Proper linkage to obstructive sleep apnea diagnoses
- Evidence of patient education and fitting
Improper billing here often leads to partial payment or denial.
Medicare Billing Considerations for Sleep Apnea Codes
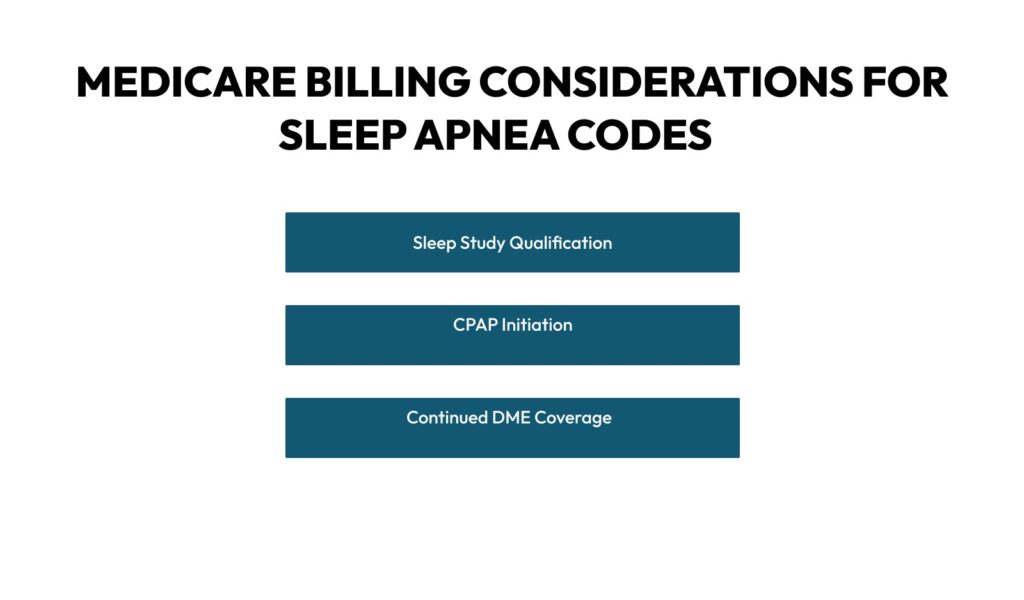
Medicare closely regulates sleep apnea services.
Coverage determinations outline strict criteria for:
- Sleep study qualification
- CPAP initiation
- Continued DME coverage
Medicare expects accurate diagnosis coding. Using G47.30 when obstructive sleep apnea has already been confirmed often leads to denials or post-payment review.
Medicare also monitors long-term CPAP compliance documentation. Diagnosis codes must align with ongoing medical necessity.
Medicaid and Commercial Payer Variations
Medicaid programs vary by state, but many require prior authorization for sleep studies and CPAP equipment. Unspecified sleep apnea codes frequently trigger requests for additional documentation.
Commercial insurers often apply automated edits to flag sleep apnea claims that lack clear diagnostic confirmation. Appeals are successful when documentation is detailed, and diagnosis coding is precise.
Practices that tailor billing workflows to payer-specific rules experience faster approvals and fewer rework cycles.
How to Avoid Sleep Apnea CPT Codes Billing Mistakes
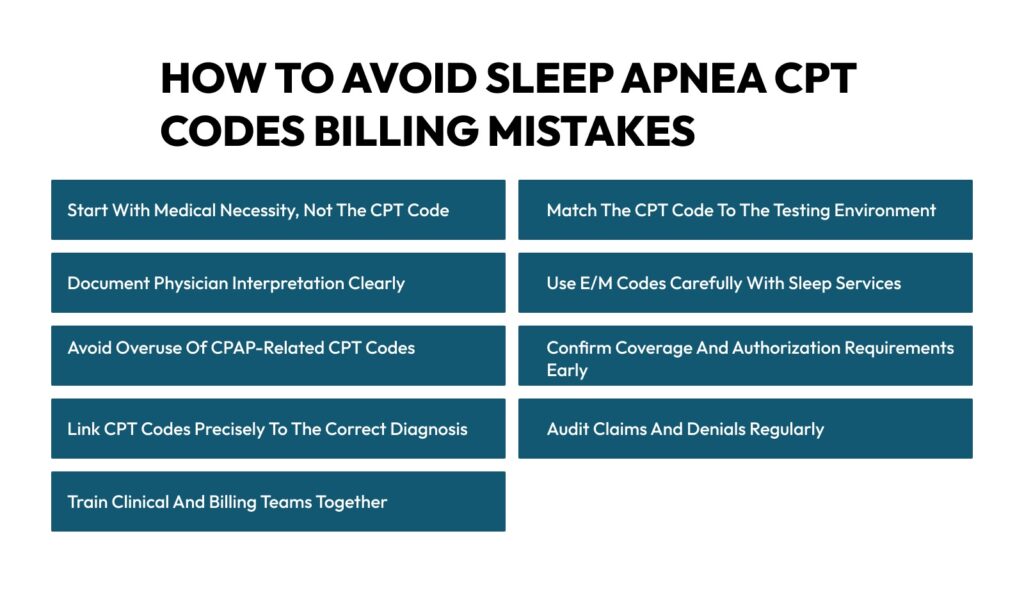
Sleep apnea billing looks simple on paper. In reality, it is one of the most closely reviewed areas in medical billing. Payers know sleep studies, CPAP therapy, and follow-up visits generate steady revenue. Because of that, they scrutinize every CPT code, modifier, and note. Small gaps often lead to denials, downcoding, or post-payment audits.
With years of revenue cycle experience in sleep medicine and pulmonary practices, most billing mistakes do not occur solely at the coding desk. They start much earlier. They begin with ordering, documentation habits, and workflow breakdowns. Let’s walk through the most effective ways to avoid sleep apnea CPT billing mistakes and protect reimbursement.
Start with Medical Necessity, Not the CPT Code
One of the biggest billing errors is choosing a CPT code first and justifying it later. Payers expect the opposite. They want to see a clear clinical story that leads naturally to the service performed.
For sleep apnea, documentation should clearly explain symptoms such as excessive daytime sleepiness, loud snoring, witnessed apneas, morning headaches, or poor concentration. Risk factors like obesity, hypertension, atrial fibrillation, or diabetes should also be clearly noted. When medical necessity is evident in the note, selecting a CPT code becomes much easier and more defensible.
Claims fail when sleep studies are billed with vague complaints like “fatigue” or “sleep issues” without a deeper clinical context. Payers often deny these claims because the testing rationale is unclear.
Match the CPT Code to the Testing Environment
Sleep apnea diagnostic CPT codes vary based on where and how the test was performed. Mixing these up is a common and costly mistake.
In-lab polysomnography codes require documentation showing why a facility-based study was necessary. Home sleep testing codes require proof that the patient met the criteria for unattended testing. Billing a home sleep test CPT code for a patient with complex cardiopulmonary disease often leads to denial, even if the test was completed correctly.
To avoid this, practices should document:
- Why in-lab testing was chosen over home testing, or vice versa
- Patient comorbidities affecting test selection.
- Ordering provider rationale
Clear justification aligns the CPT code with payer expectations and reduces pushback.
Document Physician Interpretation Clearly
Sleep study CPT codes are not just about data collection. Payers expect professional interpretation and a signed report.
One frequent mistake is submitting claims without clear documentation showing that a qualified provider reviewed and interpreted the results. Automated reports alone are not enough. The provider’s interpretation, impression, and plan must be part of the medical record.
To avoid denials:
- Ensure interpretation notes are completed before claim submission
- Include diagnosis confirmation and severity assessment.
- Clearly state the following steps, such as CPAP initiation or further testing.
This step alone prevents a large percentage of post-payment recoupments.
Use E/M Codes Carefully with Sleep Services
Evaluation and management visits are commonly billed alongside sleep apnea services. Mistakes happen when E/M levels are selected without proper medical decision-making or time documentation.
Payers expect E/M notes to reflect:
- Independent clinical assessment
- Review of sleep study results
- Treatment planning and patient counseling
Billing higher-level E/M codes repeatedly for routine CPAP follow-ups without new decision-making often raises red flags. Staying conservative and documentation-driven reduces audit risk.
When E/M services occur on the same day as diagnostic testing, correct modifier usage becomes critical. Missing or unsupported modifiers are a frequent denial trigger.
Avoid Overuse of CPAP-Related CPT Codes
CPAP-related CPT codes are among the most audited in sleep medicine. Payers closely monitor frequency and justification.
Errors often include:
- Billing CPAP assistance codes without hands-on support
- Repeating the same CPT code without documenting medical necessity
- Billing CPAP-related services without evidence of patient education or compliance review
To avoid issues, documentation should explain:
- Why was CPAP assistance required
- What support was provided
- How the service improved therapy adherence
When documentation shows real clinical involvement, claims hold up much better under review.
Confirm Coverage and Authorization Requirements Early
Many sleep apnea services require prior authorization, especially repeat sleep studies, surgical interventions, and specific advanced testing.
Billing mistakes occur when services are performed first, and authorization is checked later. At that point, payment risk is already high.
Strong front-end processes help prevent this:
- Verify payer-specific authorization rules before scheduling
- Track authorization numbers and validity dates
- Link authorizations directly to claims
This approach prevents denials that cannot be appealed successfully.
Link CPT Codes Precisely to the Correct Diagnosis
Sleep apnea has multiple ICD-10 codes. Using a generic or unspecified diagnosis often weakens the claim.
Each CPT code should clearly align with the correct diagnosis, whether obstructive, central, or mixed sleep apnea. Severity, complications, and related conditions strengthen the clinical picture and support reimbursement.
When diagnosis coding is too broad, payers question whether the CPT service was appropriate. Specificity protects the claim.
Audit Claims and Denials Regularly
Many practices repeat the same billing mistakes because no one reviews patterns. Denial trends often point directly to workflow or documentation problems.
Regular internal audits help identify:
- CPT codes are frequently denied
- Missing documentation elements
- Modifier misuse
- Authorization gaps
Fixing the root cause prevents future losses and improves overall revenue cycle performance.
Train Clinical and Billing Teams Together
Sleep apnea billing mistakes often happen because clinical staff and billing staff work in silos. Providers may not know how their documentation affects CPT selection. Billers may not fully understand clinical intent.
Joint training sessions help align both sides. When providers understand payer expectations and billers understand clinical workflows, errors drop significantly.
Why Sleep Apnea Billing Requires Specialized Expertise
Sleep apnea billing involves far more than selecting an ICD-10 code. It requires coordination between clinical documentation, diagnostic testing, CPT selection, payer policies, and long-term compliance tracking. Because sleep apnea services often include recurring testing and equipment billing, even small documentation gaps can lead to denials, delayed payments, or post-payment audits.
Medical billing teams that specialize in sleep medicine understand how diagnosis specificity, CPT pairing, and payer rules intersect. At Medhasty Medical Billing, sleep apnea billing workflows are built around payer documentation standards, diagnostic progression, and audit-resistant coding practices—helping practices reduce denials while maintaining compliance across Medicare, Medicaid, and commercial plans.
Practices that rely on generalized billing workflows often struggle with sleep apnea reimbursement. Specialized billing processes ensure that diagnosis coding, CPT services, and payer requirements remain aligned throughout the patient’s course of care.
Conclusion
ICD-10 codes for sleep apnea are not interchangeable.
Each code carries specific clinical and financial implications.
When diagnosis selection aligns with documentation, testing results, and payer rules, sleep apnea claims move smoothly through the revenue cycle. When they do not, denials and audits follow.
Precision, progression, and documentation are the pillars of successful sleep apnea billing.
FAQs
Can sleep apnea be billed without a sleep study?
In most cases, sleep apnea cannot be billed or reimbursed for treatment without objective diagnostic testing. Payers rely on sleep studies to confirm the presence, type, and severity of sleep apnea. While symptoms such as snoring, daytime sleepiness, or witnessed apneas may justify ordering a test, they rarely support payment for treatment or equipment on their own. Without documented test results, claims for CPAP therapy, oral appliances, or related services are commonly denied. Objective testing establishes medical necessity and protects the claim from audit risk.
Is G47.30 acceptable for CPAP billing?
G47.30, which represents unspecified sleep apnea, is generally not sufficient for CPAP or other durable medical equipment billing. Payers expect providers to identify whether the condition is obstructive, central, or mixed before approving therapy. Using an unspecified diagnosis often signals incomplete evaluation and increases the likelihood of denial. Updating the diagnosis once testing confirms the apnea type strengthens claims and supports ongoing treatment coverage.
Does Medicare cover home sleep apnea testing?
Medicare does cover home sleep apnea testing when specific clinical criteria are met. Coverage depends on documented medical necessity, appropriate patient selection, and proper physician interpretation. Home testing is typically approved for patients with a high likelihood of obstructive sleep apnea and without complex comorbid conditions. Claims may be denied if documentation does not explain why home testing was appropriate or if required elements, such as provider interpretation, are missing from the record.
How often should sleep apnea diagnoses be updated?
Sleep apnea diagnoses should be updated promptly once diagnostic testing confirms the type and severity of the condition. Initial suspected or unspecified diagnoses should not remain in the record once objective data is available. Updating the diagnosis ensures alignment between clinical findings, CPT codes, and payer requirements. Timely updates reduce denial risk and support continued coverage for therapy and follow-up services.
Are sleep apnea claims frequently audited?
Sleep apnea claims are subject to frequent review due to high utilization of diagnostic testing and long-term equipment use. CPAP-related services, repeat sleep studies, and DME claims receive particular attention from payers. Audits often focus on medical necessity, documentation quality, and compliance with coverage guidelines. Practices with consistent documentation and accurate coding are better positioned to withstand audits without financial disruption.
Do commercial payers follow Medicare sleep apnea rules?
Many commercial payers base their sleep apnea coverage policies on Medicare guidelines, but they do not follow them exactly. Authorization requirements, testing criteria, and coverage limits may differ by plan. Relying solely on Medicare rules can lead to denials when billing commercial insurance. Reviewing payer-specific policies and verifying requirements before testing or treatment helps avoid unexpected payment issues.