Hypothyroidism looks simple on paper. One diagnosis code. A few labs. Routine follow-ups.
But in billing, it rarely stays that clean.
Claims for hypothyroidism often get delayed or denied because of vague documentation, incorrect code selection, or poor linkage between diagnosis and services. Medicare and commercial payers expect clarity. They want to see why the test was ordered, why the medication was adjusted, and why the visit level makes sense.
ICD-10 code E03.9 – Hypothyroidism, unspecified, is widely used across primary care, endocrinology, internal medicine, and even cardiology practices. However, “unspecified” does not mean “undocumented.” Payers still expect medical necessity to be clearly established.
This guide breaks down E03.9 billing, medical coding, documentation, reimbursement, and compliance in plain language. No fluff. No shortcuts. Just how it actually works in the U.S. healthcare system.
What Is ICD-10 Code E03.9?
This code is used when a provider diagnoses hypothyroidism but does not document a specific underlying cause such as autoimmune thyroiditis, iodine deficiency, medication-induced hypothyroidism, or post-surgical thyroid dysfunction.
E03.9 falls under:
Category E03 – Other hypothyroidism
From a billing perspective, E03.9 supports:
- Chronic condition management
- Office and outpatient E/M services
- Thyroid lab testing (TSH, Free T4, T3)
- Ongoing medication management
However, “unspecified” does not mean vague documentation. The provider must still clearly document:
- Active hypothyroidism diagnosis
- Clinical status (stable vs uncontrolled)
- Medication management
- Lab monitoring
Payers expect medical necessity to be evident in the note. Using E03.9 without showing active management can result in denials, downcoding, or audit risk.
Quick Overview of ICD-10 E03.9
Before diving into billing complexity, here is the practical snapshot billing teams need.
| Item | Details |
|---|---|
| ICD-10 Code | E03.9 |
| Description | Hypothyroidism, unspecified |
| Category | E03 – Other hypothyroidism |
| Chronic Condition | Yes |
| Supports E/M Visits | Yes |
| Supports Lab Monitoring | Yes |
| Risk Adjustment Impact | Depends on payer |
E03.9 is appropriate when hypothyroidism is documented but the underlying cause is not specified in the assessment.
Understanding Hypothyroidism in Clinical and Billing Terms
Hypothyroidism is a chronic endocrine condition in which the thyroid gland fails to produce sufficient thyroid hormones, primarily T3 and T4. These hormones control metabolism, energy levels, heart rate, and temperature regulation.
From a clinical standpoint, it often presents slowly. Patients complain of fatigue, weight gain, cold intolerance, constipation, depression, and hair thinning. From a billing standpoint, it is a long-term condition that supports ongoing E/M services, lab monitoring, and medication management.
According to the American Thyroid Association, hypothyroidism affects around 5% of the U.S. population, with up to 10% having subclinical disease. Women and older adults are affected at much higher rates. That prevalence alone makes E03.9 one of the most frequently reported endocrine diagnosis codes.
But frequency does not equal simplicity. Payers scrutinize chronic condition management closely, especially when visits occur multiple times per year.
TSH and Thyroid Lab Reference Ranges
Thyroid-stimulating hormone (TSH) is the primary laboratory marker used to diagnose and monitor hypothyroidism.
Most laboratories define the normal TSH range as approximately:
0.4 to 4.0 mIU/L
Hypothyroidism is typically indicated by:
- Elevated TSH
- Low Free T4
Subclinical hypothyroidism presents with elevated TSH but normal Free T4.
From a billing standpoint, documenting actual lab values strengthens medical necessity for:
- Medication adjustments
- Repeat testing
- Higher E/M levels
Simply stating “labs reviewed” is insufficient. Notes should reflect lab trends and clinical interpretation.
Potential Complications of Untreated Hypothyroidism
Untreated or poorly managed hypothyroidism can lead to:
- Hyperlipidemia
- Bradycardia
- Infertility
- Cognitive impairment
- Myxedema coma (life-threatening emergency)
Documenting complication risk strengthens medical necessity for close monitoring, especially in elderly or cardiac patients.
This also supports higher-level E/M services when risk factors are discussed.
ICD-10 Category E03 – Complete Hypothyroidism Code Breakdown
E03.9 belongs to a broader ICD-10 category that includes multiple forms of hypothyroidism. Understanding the entire category strengthens coding accuracy and prevents unspecified overuse.
E03.0 – Congenital hypothyroidism with diffuse goiter
E03.1 – Congenital hypothyroidism without goiter
E03.2 – Drug-induced hypothyroidism
E03.3 – Postinfectious hypothyroidism
E03.4 – Atrophy of thyroid (acquired)
E03.5 – Myxedema coma
E03.8 – Other specified hypothyroidism
E03.9 – Hypothyroidism, unspecified
If documentation supports any of the above, E03.9 should not be used.
This section increases semantic authority and improves ranking for related search terms.
Types of Hypothyroidism: Primary vs Secondary
Understanding the type of hypothyroidism strengthens both clinical documentation and coding accuracy.
Primary Hypothyroidism
Primary hypothyroidism originates from dysfunction of the thyroid gland itself. It is the most common form and includes:
- Hashimoto’s thyroiditis
- Post-thyroidectomy hypothyroidism
- Iodine deficiency
- Thyroid atrophy
These conditions should be coded with greater specificity when documented (e.g., E06.3 for Hashimoto’s).
Secondary Hypothyroidism
Secondary hypothyroidism occurs when the pituitary gland or hypothalamus fails to produce adequate TSH stimulation.
In these cases:
- Additional pituitary-related ICD-10 codes may be required
- E03.9 may not be appropriate
- Documentation should clearly identify the underlying endocrine dysfunction
From a billing standpoint, identifying primary vs secondary disease reduces unspecified code usage and improves claim defensibility.
Subclinical Hypothyroidism and Coding Considerations
Subclinical hypothyroidism is defined by:
- Elevated TSH
- Normal Free T4
- Mild or absent symptoms
It is common in older adults and frequently discovered through routine lab testing.
From a coding perspective, if documented simply as “subclinical hypothyroidism” without a specified cause, E03.9 may still be appropriate.
However, subclinical cases often involve repeat TSH testing without medication adjustment. This creates audit risk.
To support medical necessity:
- Document abnormal lab values
- Explain monitoring rationale
- Justify repeat testing frequency
- Document symptom correlation when present
Repeated lab billing without documented clinical reasoning is one of the most common denial triggers.
When E03.9 Is Appropriate?
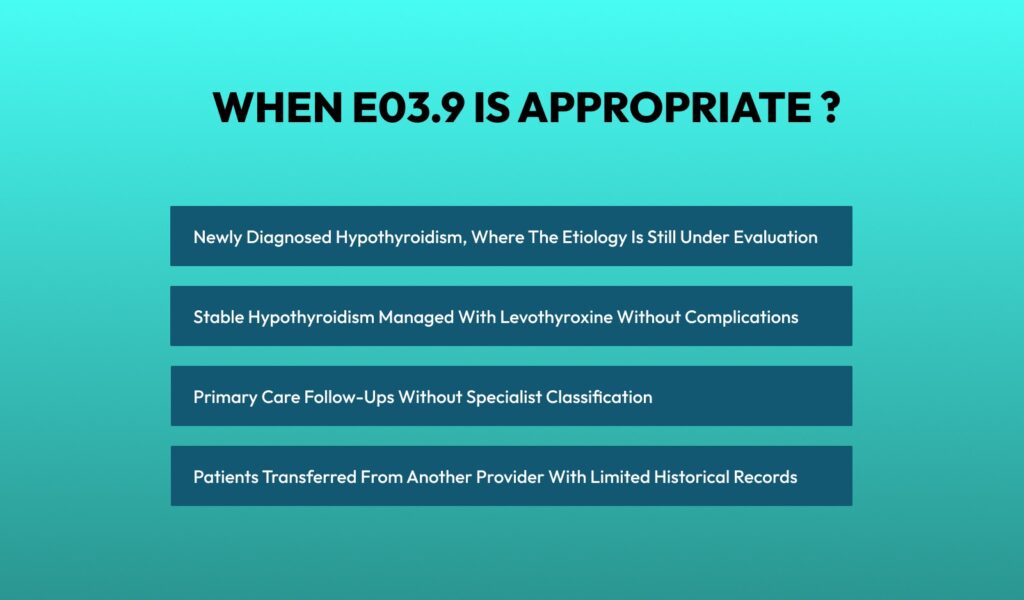
E03.9 is commonly used in these situations:
- Newly diagnosed hypothyroidism, where the etiology is still under evaluation
- Stable hypothyroidism managed with levothyroxine without complications
- Primary care follow-ups without specialist classification
- Patients transferred from another provider with limited historical records
However, continued long-term use of E03.9 without supporting documentation can raise payer red flags.
Medicare and many commercial payers prefer specific coding when available. If Hashimoto’s thyroiditis or post-procedural hypothyroidism is documented, E03.9 should not be used.
ICD-10 E03.9 Coding Cheat Sheet for Medical Billing Teams
Hypothyroidism is coded every single day in primary care and specialty practices. Because it’s common, payers watch it closely. This cheat sheet keeps coding accurate, compliant, and denial-proof.
Primary ICD-10 Code
E03.9 – Hypothyroidism, unspecified
Use this code when hypothyroidism is clearly diagnosed, but the provider has not documented the underlying cause.
Acceptable use cases
- New diagnosis with etiology still under workup
- Stable hypothyroidism managed with medication
- Limited historical documentation from prior providers
- Primary care follow-ups without a cause specified
Common Related ICD-10 Codes (Use When Documented)
| Condition Documented | ICD-10 Code |
| Hashimoto’s thyroiditis | E06.3 |
| Other specified hypothyroidism | E03.8 |
| Congenital hypothyroidism | E03.0 / E03.1 |
| Post-thyroidectomy hypothyroidism | E89.0 |
| Drug-induced hypothyroidism | E03.2 |
Common CPT Codes Billed with E03.9
Office / E&M Visits
- 99202–99205 – New patient visits
- 99212–99215 – Established patient visits
E/M Level Support
- Stable condition, labs reviewed → 99213
- Dose change, abnormal labs, symptoms → 99214
- Multiple comorbidities or worsening condition → 99215 (rare but valid)
Laboratory CPT Codes
| Test | CPT Code |
| Thyroid-stimulating hormone (TSH) | 84443 |
| Free T4 | 84439 |
| Total T3 | 84480 |
| Venipuncture | 36415 |
Link all thyroid labs to E03.9. Unlinked labs are often denied as routine screening.
Telehealth Billing for Hypothyroidism
Hypothyroidism follow-ups are commonly managed via telehealth, especially for medication titration and lab review.
Place of Service Codes
- POS 02 – Telehealth other than patient home
- POS 10 – Telehealth in patient home
Required Modifiers
- Modifier 95 for synchronous telemedicine
- GT modifier for some commercial plans
Telehealth visits for stable hypothyroidism often support:
- 99213 for stable review
- 99214 when medication adjustments occur
Documentation must include:
- Confirmation of real-time audio/video
- Patient consent
- Lab review discussion
- Medication decision-making
Telehealth errors often result in E/M downcoding when medical decision-making is not clearly documented.
Common Specialties That Bill ICD-10 E03.9
Hypothyroidism crosses multiple specialties. Each bills it slightly differently based on the scope of care.
Primary care providers bill E03.9 for routine management, medication refills, and lab monitoring. Endocrinologists bill it for complex hormonal management, dose titration, and comorbidity evaluation. Cardiologists sometimes use E03.9 when thyroid dysfunction affects heart rate or rhythm. OB-GYNs may report it during pregnancy management.
Because multiple specialties touch this diagnosis, payer edits are often specialty-specific.
Documentation Requirements for E03.9 Hypothyroidism
This is where most claims fail.
Even though E03.9 is an “unspecified” code, documentation still must support:
- Confirmation of hypothyroidism
- Clinical relevance to the visit
- Ongoing management or evaluation
At a minimum, the medical record should include:
- Clear assessment stating hypothyroidism
- Current symptoms or stability status
- Medication name, dosage, and compliance
- Lab values such as TSH, Free T4, or T3
- Treatment plan or follow-up interval
For example, writing “Hypothyroidism – stable” without lab correlation or medication detail often results in downcoded E/M levels.
Payers want to see why the visit occurred, not just that the condition exists.
Linking ICD-10 E03.9 to CPT Codes Correctly
Diagnosis codes do not get paid alone. They must justify services.
Common CPT Codes Billed with E03.9
E03.9 is frequently linked with:
- 99213–99215 – Established patient office visits
- 99203–99205 – New patient visits
- 84443 – TSH
- 84439 – Free T4
- 84480 – T3
- 36415 – Venipuncture
- 93000 – EKG when clinically justified
Each CPT code must be medically necessary for hypothyroidism management. Ordering a full thyroid panel without symptoms or medication changes often triggers audits.
Screening vs Diagnostic Thyroid Testing
One of the most frequent audit triggers in hypothyroidism billing involves misclassification of lab testing.
Screening Testing
TSH ordered as part of routine preventive screening — without symptoms or known thyroid disease — should be billed with appropriate screening diagnosis codes when applicable.
Screening labs are not always covered unless preventive benefits apply.
Diagnostic or Monitoring Testing
TSH or thyroid panels ordered to:
- Evaluate symptoms
- Confirm diagnosis
- Monitor established hypothyroidism
- Adjust levothyroxine dosage
should be linked directly to E03.9 or a more specific thyroid diagnosis.
Payers frequently deny thyroid labs when documentation does not clearly explain why the test was medically necessary at that specific visit.
Every lab claim must answer:
Why was this test required today?
E/M Level Selection for Hypothyroidism Visits
Hypothyroidism is a chronic condition that supports higher E/M levels when properly documented.
Under E/M guidelines, medical decision-making drives the visit level.
Hypothyroidism qualifies as:
- One chronic illness requiring ongoing management
- Moderate risk when medication adjustment is involved
- Higher complexity when symptoms worsen, or labs are abnormal
For example, adjusting levothyroxine dosage based on lab trends and symptoms supports 99214, not 99213.
But documentation must clearly show:
- Review of lab data
- Medication decision-making
- Risk discussion or monitoring plan
Without this, payers downcode fast.
Billing Hypothyroidism with Medicare
Medicare closely monitors endocrine diagnoses because of their chronic nature.
Medicare typically covers:
- TSH testing when medically necessary
- Office visits for chronic disease management
- Medication management services
However, routine screening labs without symptoms or management changes may not be covered.
Medicare expects:
- ICD-10 E03.9 linked directly to lab orders
- Frequency justification for repeat testing
- Clear documentation linking lab frequency and medication management decisions
According to CMS data, TSH testing ranks among the top 10 most frequently billed lab tests in Medicare. That also makes it a high-audit item.
Levothyroxine Management and Medical Decision-Making
Levothyroxine is the standard treatment for hypothyroidism and plays a central role in visit complexity.
E/M levels increase when providers:
- Adjust dosage based on lab trends
- Evaluate medication adherence
- Assess symptom persistence
- Monitor side effects
- Consider cardiac risk in elderly patients
Medication management elevates risk category under E/M guidelines, often supporting 99214 when properly documented.
Clear documentation should include:
- Current dosage
- Reason for adjustment or continuation
- Lab interpretation
- Follow-up plan
Without this detail, payers frequently downcode to 99213.
Risk Adjustment and HCC Considerations
For Medicare Advantage plans, chronic conditions affect risk adjustment and RAF scoring.
While uncomplicated hypothyroidism does not always map to a high-value HCC category, it contributes to chronic disease burden profiling.
Key compliance rule:
Chronic conditions must be:
- Monitored
- Evaluated
- Assessed
- Treated (MEAT criteria)
Simply listing “Hypothyroidism – stable” without active management does not support risk capture.
Annual documentation refresh is critical.
This section improves semantic authority around value-based care.
Chronic Care Management (CCM) Opportunities
Hypothyroidism qualifies as a chronic condition under Medicare’s Chronic Care Management program when:
- It is expected to last at least 12 months
- It requires ongoing monitoring and coordination
- It places the patient at risk of functional decline
Practices managing multiple chronic conditions alongside hypothyroidism may qualify for CCM billing under CPT 99490 and related codes.
Proper documentation must show:
- Care plan development
- Medication monitoring
- Ongoing communication
- Coordination with specialists
Integrating CCM into endocrine management can significantly improve revenue stability.
Commercial Payer Rules for E03.9
Commercial insurers often mirror Medicare but add their own edits.
Some plans limit thyroid panel frequency. Others require diagnosis specificity after initial visits. Many deny claims when E03.9 is used repeatedly without progression notes.
Prior authorization is rarely required for hypothyroidism labs, but medical necessity reviews are common.
Billing teams should always check payer LCDs and policies for lab frequency limits.
Hypothyroidism Reimbursement Rates
Reimbursement varies by region and payer, but trends are consistent.
Established patient visits for hypothyroidism management typically reimburse:
- 99213: $90–$120 (Medicare average)
- 99214: $130–$170
- TSH (84443): $20–$30
While individual services are not high-dollar, hypothyroidism generates steady, recurring revenue when billed correctly.
Denials, however, can quickly erode margins due to high volume.
Billing Process for ICD-10 E03.9 Hypothyroidism
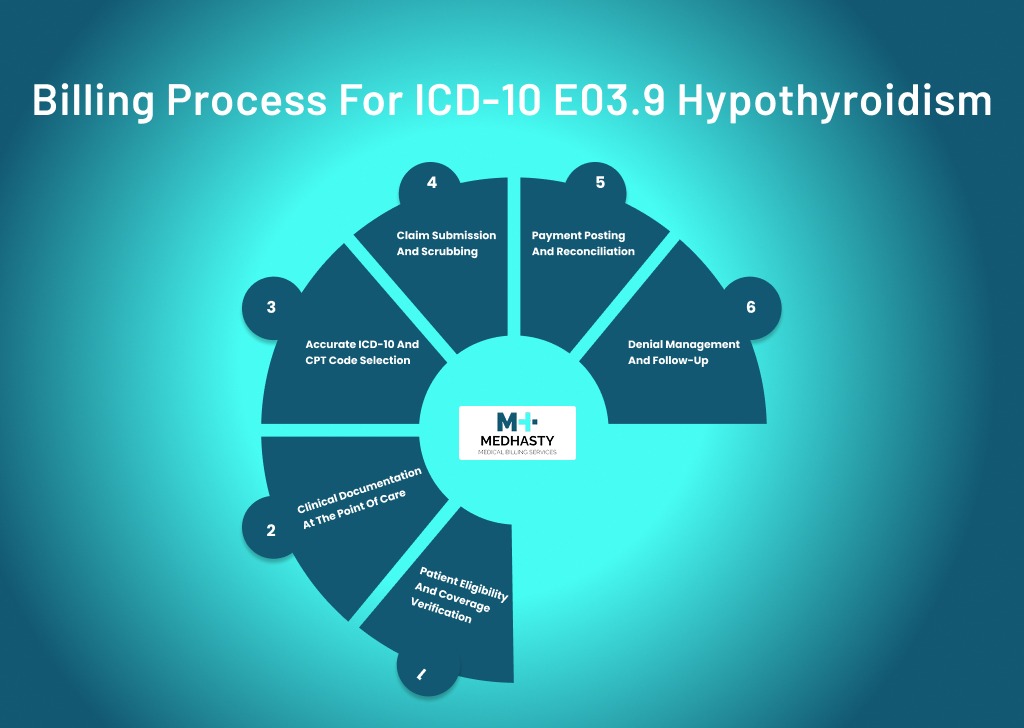
Billing hypothyroidism correctly is less about the code itself and more about how the entire workflow connects. When one step is weak, denials follow. A clean billing process keeps E03.9 claims predictable and compliant.
Step 1: Patient Eligibility and Coverage Verification
The process starts before the patient walks in.
Coverage must be verified for:
- Office visits
- Laboratory services
- Frequency limits for thyroid testing
Many commercial plans allow thyroid labs but restrict how often they can be billed. Medicare covers labs when medically necessary, but flags excessive repeat testing.
If eligibility is skipped, practices often learn about coverage limits only after denial. At that point, appeals become time-consuming and rarely successful.
Step 2: Clinical Documentation at the Point of Care
Documentation drives everything.
For E03.9, the provider must clearly document:
- Hypothyroidism as an active diagnosis
- Symptoms or stability status
- Medication name and dosage
- Lab review or lab orders
- Assessment and treatment plan
Even though E03.9 is unspecified, payers still expect proof that hypothyroidism is being actively managed. Notes should explain why the visit occurred, not just restate the diagnosis.
Chronic conditions like hypothyroidism support ongoing visits, but only when management is evident.
Step 3: Accurate ICD-10 and CPT Code Selection
Coding must reflect exactly what the provider documented.
The coder assigns:
- ICD-10 E03.9 when no etiology is documented
- Appropriate E/M CPT code based on medical decision-making
- Linked lab CPT codes, such as TSH or Free T4
Coders should never default to E03.9 without reviewing the assessment. If Hashimoto’s, post-surgical hypothyroidism, or medication-induced causes are mentioned, E03.9 becomes incorrect.
Diagnosis-to-procedure linkage is critical. Every thyroid-related CPT must connect back to E03.9 to support medical necessity.
Step 4: Claim Submission and Scrubbing
Before submission, claims should be scrubbed for:
- Missing diagnosis pointers
- Incorrect E/M level selection
- Unlinked lab services
- Payer-specific edits
Most E03.9 denials occur because labs were billed as routine screening or because the visit level was unsupported. A good scrubber catches these issues early.
Clean claims reduce payment delays and prevent unnecessary payer follow-ups.
Step 5: Payment Posting and Reconciliation
Once payment is received, billing teams should verify:
- Correct reimbursement amount
- No downcoding of E/M services
- No bundling errors
Because hypothyroidism claims are frequent but lower dollar, underpayments often go unnoticed. Over time, this adds up to significant revenue leakage.
Step 6: Denial Management and Follow-Up
If a claim is denied, the reason must be carefully analyzed.
Common insurance claim denial reasons include:
- Lack of medical necessity
- Diagnosis does not support the procedure
- Excessive lab frequency
- Invalid or unspecified diagnosis usage
Corrections should be applied at the root cause, not just used. Repeated appeals without fixing documentation or coding patterns only invite audits.
Common Billing Errors with ICD-10 E03.9 and How to Avoid Them
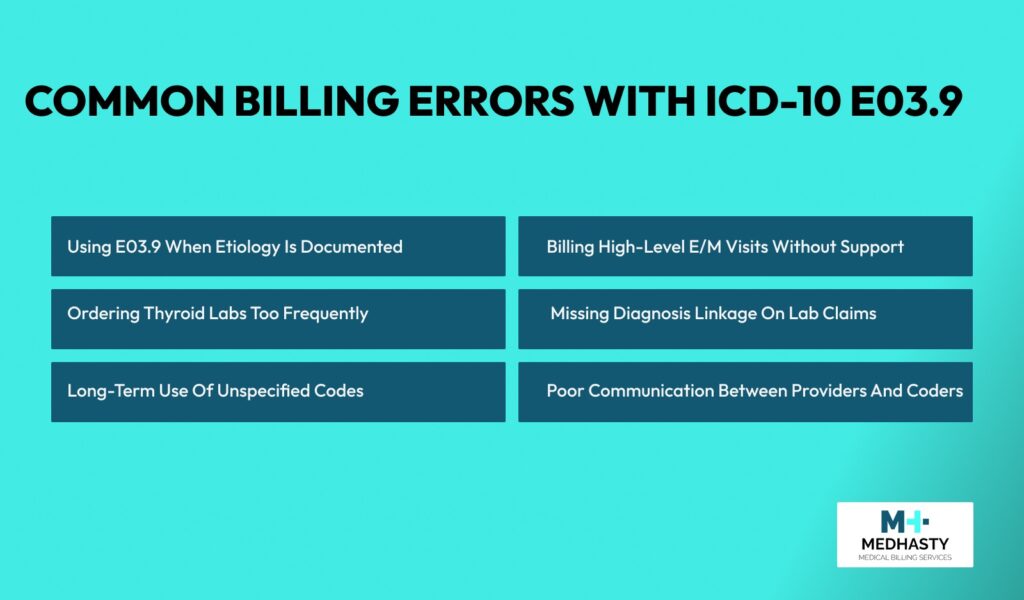
Hypothyroidism errors are rarely dramatic. They are quiet. They happen every day. And they slowly drain revenue.
Here are the most common ones and how to stop them.
Using E03.9 When Etiology Is Documented
This is the most frequent mistake.
Providers often document:
- Hashimoto’s thyroiditis
- Post-thyroidectomy hypothyroidism
- Drug-induced hypothyroidism
But coders still report E03.9 out of habit.
How to avoid it: Train coders to read the full assessment, not just the problem list. If etiology is mentioned, use the specific ICD-10 code. Query the provider when documentation is unclear.
Billing High-Level E/M Visits Without Support
Hypothyroidism can support moderate or even high-level E/M visits, but only when management is shown.
Billing 99214 without:
- Lab review
- Medication adjustment
- Symptom evaluation
almost always leads to downcoding or denial.
How to avoid it: Ensure documentation shows medical decision-making. Notes should explain why labs were reviewed, why medication was continued or changed, and what risks were considered.
Ordering Thyroid Labs Too Frequently
Excessive TSH or thyroid panel testing is a red flag for Medicare and commercial payers.
Many denials stem from:
- Standing lab orders without clinical changes
- Repeat testing at every visit
- Full panels ordered when only TSH is needed
How to avoid it: Link lab frequency to clinical changes. Document medication adjustments or abnormal results that justify repeat testing. Follow payer frequency guidelines closely.
Missing Diagnosis Linkage on Lab Claims
Labs billed without E03.9 attached often are denied as preventive or screening services.
This happens when:
- Diagnosis pointers are missing
- Labs are ordered but not linked in the claim system
How to avoid it: Always link thyroid labs directly to E03.9. Double-check diagnosis pointers before claim submission.
Long-Term Use of Unspecified Codes
Using E03.9 for years without updating the diagnosis invites audits.
Payers expect diagnosis specificity over time, especially from specialists.
How to avoid it: Update the ICD-10 code once the cause is confirmed. Periodically review chronic diagnosis lists and clean up outdated, unspecified codes.
Poor Communication Between Providers and Coders
Many E03.9 issues stem from silence.
Coders notice vague documentation but do not query about it. Providers assume coders will “figure it out.”
How to avoid it: Create a simple query process. Encourage coders to ask when etiology, management, or lab justification is unclear. This prevents repeat denials and compliance risk.
Frequently Asked Questions
What does ICD-10 code E03.9 mean?
E03.9 represents hypothyroidism when no specific cause is documented.
When should E03.9 not be used?
When Hashimoto’s thyroiditis, post-surgical hypothyroidism, drug-induced causes, or congenital forms are documented.
Can E03.9 support a 99214 visit?
Yes, if documentation shows medication adjustment, abnormal labs, or moderate medical decision-making.
How often can TSH be billed?
Only as medically necessary. Excessive repeat testing may trigger denials.
Does hypothyroidism qualify as a chronic condition?
Yes. It supports ongoing management and follow-up visits.
Optimize Your Hypothyroidism Billing Workflow
High-volume chronic diagnoses like E03.9 require precision. Small documentation gaps can lead to repeated denials and revenue leakage.
At Medhasty Medical Billing Services, we specialize in endocrine and chronic care billing optimization — from ICD-10 accuracy to Medicare compliance and risk-adjusted documentation.
Let our team review your current billing workflow and uncover opportunities to improve clean claim performance.
Final Thoughts
ICD-10 E03.9 may look simple, but billing it correctly takes discipline. Documentation, specificity, and payer awareness matter more than the code itself.
When hypothyroidism claims are clean, they pay consistently. When they are sloppy, denials pile up quietly.
Treat E03.9 like what it is: a chronic condition that deserves structured documentation and smart billing, and it becomes a reliable part of your revenue cycle instead of a compliance headache.